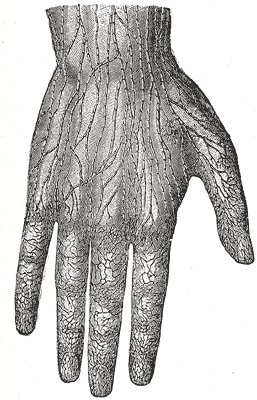
Fascia: The Body’s Transmission System
We spend a lot of time talking about the nervous system and how it controls what we’ve done. And, being a chiropractor, I really do appreciate its importance. But I’ve always asked myself, what if there’s more to the story? Nerves have to function digitally, with action potentials that only fire in an “all-or-nothing” pattern, […]
Why You Need to Start Dead Hanging
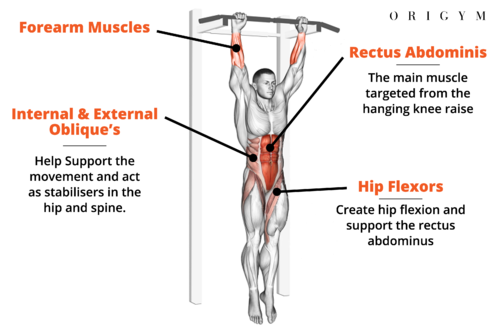
Why You Need to Start Dead Hanging Welcome aboard the dead hang express, where hanging from a bar isn’t just a workout—it’s a game-changer for your daily life! Here’s why you should join the hanging revolution: Chlorine in Drinking Water: Why This is a Problem Since the 1800s, chlorine has been the go-to solution for […]
Building a Better Brain

Happy belated Mother’s Day to all the mothers out there! My mom has been an irreplaceable part of my life, and I don’t know if I’d be where I am today without her support. I will also soon be a father myself, and I was really excited to celebrate the day with my wife as […]
Nasal Breathing 101: What Is Disordered Breathing?
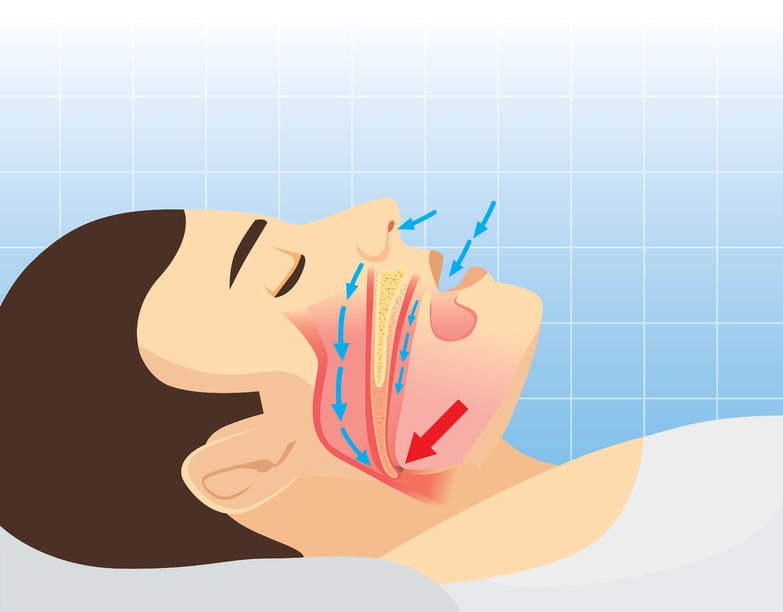
How Do You Breathe? On the face of it, it sounds like a ridiculous question. But the truth of the matter is most folks aren’t doing the best they can, and the numbers are getting worse. Sleep apnea cases are on the rise, about 1 in 12 Americans suffer with asthma, and over 100 million […]
Acids & Bases: Understanding pH, Redox, and Your Health
This week, I hope to blend some of the physics we’ve been learning with chemistry. This is because, at the root of it all, living systems exist due to negative entropy. This blog post would be a good refresher. This is done through motion and flow at the quantum level. Very few people, like Fritz […]
The Road to Better Health, Part 1: Spirit
Welcome! Because you’re here, you are now traveling on the road to better health! This process is here to guide you through creating a healthy body, mind, and spirit, one step at a time. It doesn’t matter where you are on your healing journey! There is something here that anyone can employ. Simply follow the […]
Tend to Your Terrain! (Understanding Your Microbial Ecosystem)

The concept of bacteria in our gut affecting overall human metabolism (and by extension, our weight and overall health) has only been around for about a decade or so, but ancient healing arts have referenced this concept in other ways through the years. Nature is fractal. Each cell is a microcosm of the whole that […]
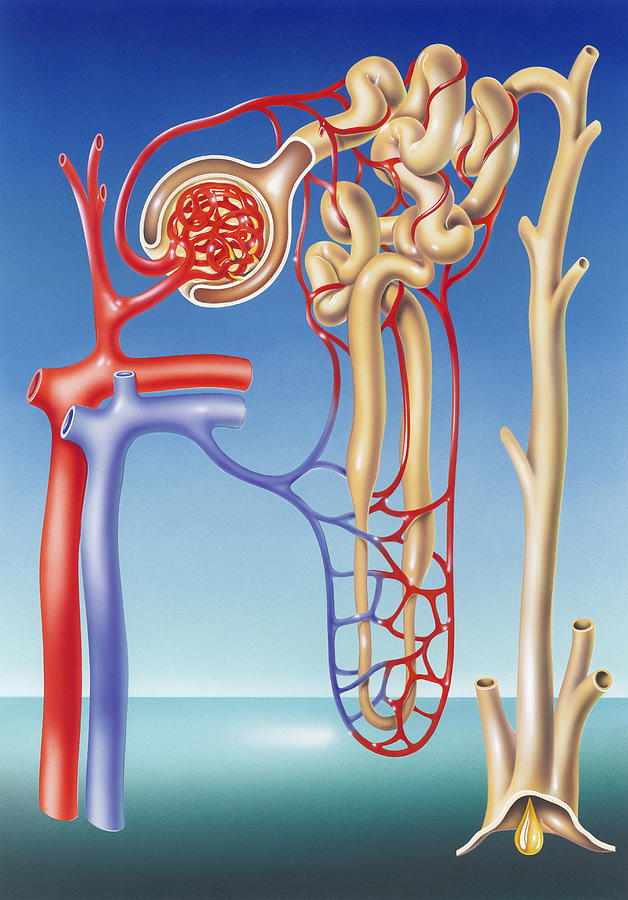
Your Body Is Amazing Part 5: Cell Healing, Redox, & Detox Pathways
We are made up of almost 40 trillion cells and about 100 trillion more bacteria, fungi, and other microbes that make up the microbiome. It is more accurate to say that the body is an ecosystem composed of many different types of cells that work together rather than an individual organism. If you just add […]