I’ve never suffered from plantar fasciitis personally until now. But I’ve worked with other people to help them fix their own foot pain. Sometimes it can be stubborn, and patience is required. Usually though, you can see real improvement in a few short weeks and months, with consistency.
Turns out, between 11-15% of adults experience plantar fasciitis, which is sometimes called plantar heel pain (PHP). Whether you’re experiencing symptoms yourself or simply looking to learn more, let’s talk about what plantar fasciitis is and what you can do about it from the comfort of your own home.
What is Plantar Fasciitis?
Plantar fasciitis develops when the plantar fascia, a thick band of tissue spanning the underside of the foot, becomes inflamed or irritated. It is identified by pain and stiffness in the heel and/or arch of the foot, which can make it uncomfortable to stand and walk for extended periods of time.
Some of the common symptoms include:
- Dull or sharp pain in the heel and/or arch of the foot, fluctuating in intensity
- A burning or stabbing pain sensation
- Additional discomfort following extended periods of standing or walking
- Foot stiffness and tenderness that hampers movement
- Presence of a lump or knot in the arch of the foot
- Clicking or popping sensation in the foot
There are almost always multiple factors that play a role in the development of plantar fasciitis, some of which can include:
- Repetitive stress on the plantar fascia from activities like running, jumping, or prolonged standing on hard surfaces with poor footwear
- Tight Achilles tendon
- Weakness in the gastrocnemius or soleus muscles on the same leg
- Weakness in the hip abductors on the opposite leg
- Low back imbalances
- Weakness in the intrinsic foot muscles
- Structural distortions of the foot, like flat feet or high arches, increase strain on the plantar fascia
- Obesity or rapid weight gain, imposing extra pressure on the feet and worsening preexisting foot issues
- Having a job where you are standing on hard surfaces, floors, hardwood, cement etc.
- Exercising with poor form on hard surfaces
- Muscle imbalances (weakness) in the lower body kinetic chain, from the low back, hip, knee, ankle, etc.
- Inflexibility of the ankle, knee, hip, lower back, and generally poor alignment/tracking
- Starting an exercise program or physically demanding job too quickly without giving the feet time to adjust
- New shoes, particularly shoes with narrow toe boxes
- History of inflammatory health ailments like diabetes, tarsal tunnel syndrome, arthritis, etc.
While it can be painful and uncomfortable, there are many healing modalities available to promote a smooth recovery.
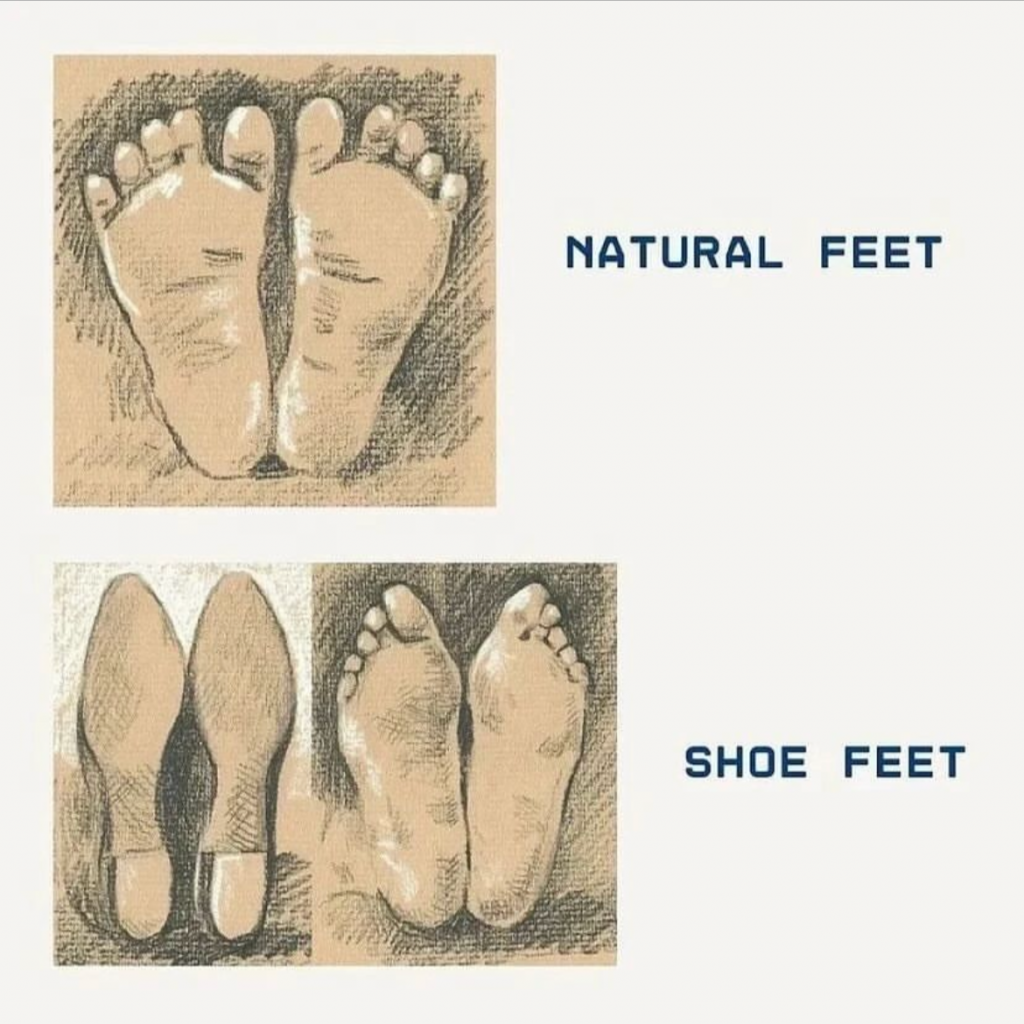
Improper footwear and weak intrinsic foot muscles are real problems for Modern Humans. Evolution through thousands of generations created human feet that are able to endure walking and running barefoot on natural surfaces. This has changed dramatically in the past sixty-plus years.
Born to Run (and Walk)
Modern humans spend most of their time (over 90%) indoors on hard, flat surfaces. They are also spending most of that time sedentary, perhaps with the odd short bouts of intense exercise.
This is much different than the consistent, moderate movements humans have done for thousands of years. Due to the cultural modern norms, we block our exercise into small time intervals. Unlike our predecessors, it is not spread out over the hours we are awake.
For context, the best estimates we have say that ancient humans walked 10,000-18,000 steps per day! Modern humans walk, on average, less than 1.5 miles per day. For those of you that count steps, 1 mile is about 2000 steps for adults. To add insult to injury, the Modern Human sits for 6-8 hours per day (based on 2010-2013 data; I’d imagine this number has only gone up).
Benefits of Walking
This is unfortunate because regular, low-intensity walking under the influence of gravity is one of the most effective regenerative treatments known to humans.
According to the Harvard School of Public Health, walking just one to two miles a day lowers blood pressure and decreases risk of stroke by 40%.
Walking, especially walking outdoors, strengthens bones. Walking stops the loss of bone mass and decreases risk of hip fractures by 40%. We also now know that walking 6-9 miles per week also slows down age-related memory decline and lowers dementia and Alzheimer’s risk.
Walking is a well-known mood-lifter. The more steps you take, the better your mood tends to be! Walking releases natural pain-killing endorphins to the body.
Another nice benefit is a longer life! Individuals who maintain a regular exercise regimen in their fifties and sixties have a 35% lower risk of mortality over the subsequent eight years compared to those who do not engage in physical activity. For people with underlying health conditions, the likelihood of mortality decreases by 45%.
Current Day
Human physiology is uniquely suited for endurance movement, like running, evidenced by our ability to sweat to regulate body temperature, strong hip muscles, short parallel toes, straight legs, and elongated tendons compared to other primates.
From an evolutionary perspective, we know that humans have been running long distances for over 2 million years and the adaptations to our anatomy and physiology stimulated by endurance running are what separate us from our closest primate cousins. Also, keep in mind that the earliest sandals and moccasins did not exist until about 40,000 years ago.
Healthy Feet
For plantar fasciitis to heal, you need healthy feet. You want to build strong and stable feet that can manage walking on natural surfaces.
Walking is a dynamic movement. Like all body movements, there is no individual muscle or joint that is most important. The body is an integrated unit. In the case of injuries, all other joints in the kinetic and fascial chains should be examined as well. Right now, the science of healthy walking the foot has 3 ‘rockers’:
- Heel rocker
- Ankle rocker
- Forefoot (big toe) rocker
Much of our ability to walk is determined by how well these rockers function together. Human feet are designed to push off from the ball and big toe. Biomechanically, this is where we generate the most leverage.
The foot also serves as our foundation, or support base. The foot support is made up of three primary arches:
- Medial longitudinal arch
- Lateral longitudinal arch
- Anterior transverse arch
The arches function like springs. When loaded, they allow for elastic recoil as the arch collapses. When they are not bearing weight, the intrinsic muscles and ligaments offer arch support.
This elasticity is vital. When running, the body must absorb shock equal to twice its own weight. 52% of that shock absorption occurs in the arches and the ankle. However, you take away this shock absorption mechanism with heel striking, transferring more of the shock load to the knees and hips.
Do Flat Feet or High Arches Matter?
Interestingly, a study found that arch height made no difference in pain or function of the foot.
Many people with low or high arches will never really notice it. However, if there is an issue with the arches, then there is a risk that you will have issues with absorbing impact and providing spring-like rebound necessary for healthy walking and running.
In a minority of cases, excessively low or high arches can disrupt foot function. If you belong to this group, you’re likely already familiar with these challenges.
Today, most people have heard that they should seek support, get custom orthotics, or specially designed shoes. Of course, these options will leave you with your pockets feeling a bit lighter.
The best evidence today suggests that custom orthotics make no significant difference statistically as far as providing any benefit. The study examined a group of children with flat feet. These children were given orthotics to wear for a few weeks, and saw no significant difference in outcomes.
What IS interesting, though, is that we do have evidence that clearly shows exercising and strengthening the intrinsic foot muscles statistically improved outcomes. It is worth noting that these researchers also found that orthotics did not help.
This makes a lot of sense to me. The feet are made up of many muscles, tendons, bones, and ligaments. Strengthening and mobilizing these tissues should improve functionality.
In other words, it isn’t about providing support with custom shoes and orthotics. They are the equivalent of crutches. Perhaps they can provide some benefit short-term, but they will not make your life easier over time.
The true remedy is not putting your foot in a cast, which is basically what an orthotic does. It is making the foot itself stronger.
As Dr. Benno M. Nigg, an orthotics researcher, states, “The idea that [orthotics] are supposed to correct mechanical-alignment problems does not hold up.”
Orthotics may be necessary if the foot is distorted such as cases of malformation or people that have had some toes removed. However, for the standard foot, orthotics should be eliminated once the normal biomechanics of the foot are restored.
The Shoes You Wear
The goal of most modern footwear is to manipulate natural foot movements through two predominant “technologies”: motion control and shock absorption.
These “technologies” have led to generations of shoes that encourage poor foot mechanics for their users. Consistently using your feet in an unnatural way is likely going to lead to more injuries, particularly in the lower extremities. This is why, despite sixty years of modern shoe design, there is no evidence that underfoot technologies reduce the incidence of foot injuries.
As an analogy, think of this as a computer problem. You have hardware and software. We clearly see alterations in software (movement patterns) and hardware (body and foot shape) are evident when comparing people who walk around predominantly barefoot versus the conventional shoe wearer.
Feet that are constantly in shoes tend to have weaker intrinsic muscles, ligaments, and a diminished plantar fascia. When the foot arch collapses, the muscles and tendons have less of an ability to recoil, which can lead to an injury.
Common foot problems today are Morton’s Foot and bunions. Morton’s Foot is where the big toe has receded behind the second toe, and a bunion is a reformation of the big toe. These are often encouraged and exacerbated by poor shoe design.
Where Are Your Feet?
When you wear the common modern-day shoe, with all of its padding and support, you are sending different signals to the brain. Removing sensory feedback via padded shoes hampers the brain’s ability to generate appropriate movements, resulting in awkward walking and running patterns.
Proprioception is the body’s ability to sense movement, location, and action in space. There are three main systems that play a role in proprioception:
- The vestibular system: located in the ear; sends information about rotational movements, position, and acceleration in space
- Eyes: relay visual information
- Stretch receptors: found in every muscle, in skin, and in joints; they relay information about the position of body parts in space.
- Brain: responsible for receiving and interpreting information relayed from the vestibular system, eyes, and stretch receptors
Without proprioception, you wouldn’t be able to move without thinking about your next step. A neurological test many health practitioners will ask their patients to perform is to have said patient close their eyes and touch their nose with their index finger. If the patient misses the nose or looks uncomfortable getting there, it could tip off the practitioner that there is something wrong neurologically or with proprioception.
Proprioception is inhibited by wearing the modern-day shoe. This results in less coordinated movements and can result in injury. Running and walking are complex movements comprising various motor skills. Just as a baby learns to sit before crawling, standing, and walking, re-learning natural movement requires a step-by-step approach.
Skilled walking and running relies on three fundamentals:
- Posture: should be upright, neck tall, and allowing for proper spinal curves
- Rhythm: leg cadence should be even from step to step. You should be able maintain consistent stride lengths and tempo whether walking or running
- Subconscious Movement Patterns: Movement is ultimately subconscious. This is why if you have trained poor movement patterns, you may have to actively relearn healthier movement patterns to improve foot conditioning.
Many folks tend to focus on foot-strike, but the truth is how the foot strikes will change depending on if you are walking or running. It becomes inconsequential when these fundamentals are in place.
Are Barefoot Shoes Good for Flat Feet?
Short Answer: Yes.
Long Answer:
Footwear is extremely important because most shoes don’t allow for proper motion of the feet. Going barefoot as often as possible is best, but if you don’t live in an environment that allows you to walk barefoot then you’ll want to invest in the proper footwear. My favorite site that reviews all the best brands is called Anya’s Reviews.
Barefoot shoes are a fantastic idea for people with flat feet or for people who want to move more naturally and promote muscle strengthening for enhanced support. They prioritize natural foot movement.
Unlike most modern footwear, they feature thin, flexible soles that allow for safe ground feel and zero drop, meaning they don’t slope from heel to toe. Additionally, barefoot shoes typically offer a spacious, foot-shaped toe box, allowing plenty of room for toe movement. They can be great for running (eventually) as well.
Again, logically, people have been walking and running with minimalist footwear for thousands of years, if they had any shoes at all. Walking or running with a little protection (or even bare feet when appropriate) allows for greater activation of the foot muscles. You simply do not get this muscle activation in most modern-day footwear.
“Normal” shoes have thick soles with lots of support and cushioning. They limit movement of the feet. If you add in a rigid arch support, that will limit movement even more. And, as this study supports, if you’re not working the muscles of the foot because you’re using orthotics, they eventually will get weaker.
So the concept of barefoot shoes being helpful isn’t based on some wild theory. It’s just getting back to Nature. One study found that just walking in minimalist shoes can strengthen foot muscles to a similar extent as dedicated foot strengthening exercises. Another found that using barefoot or minimalist shoes improved muscle strength and foot arch stiffness.
Remember, this isn’t medical advice. Sometimes, at least early on, those with plantar fasciitis may need more support to walk on hard surfaces, and that’s fine (although, I must say having shoes with a wide to box is incredibly beneficial). However, your long-term goal should be to strengthen your feet and recreate barefoot walking with minimalist shoes or barefoot as much as you can, when tolerable.
But I am encouraging you to at least consider the possibility that you can build healthy feet wearing barefoot shoes if you have plantar fasciitis or flat feet — even if you’ve assumed you would always need “comfortable” and “supportive” traditional shoes.
The best types of shoes are ones that have absolutely no arch support and allow full motion of the foot. They are essential for people that have been wearing orthotics. It just may take some time to adjust.
If you are in the market for exercise shoes, you absolutely want to consider ones with wide toe boxes. You should be able to wiggle your toes. Depending on the terrain and sport, your shoes should have a strong sole that flexes at the ball of your foot.
Working with a Professional
If you are going to work with a doctor, make sure he/she is well-versed in natural movement patterns and wants to encourage that as an end-goal. Having an arch support or more cushioned shoes are not solutions.
If you decide to work with a provider, here is what you should expect:
- During either an in-person or virtual exam, your healthcare provider is likely to examine your feet thoroughly. A good one will ask you to stand and walk to assess your gait and foot structure.
- The provider should ask you to describe your symptoms, their timing, and any activities or factors that alleviate or exacerbate the discomfort
- Sometimes, depending on the presentation, the provider may ask you to get imaging tests like X-rays or MRIs to rule out other conditions
- Once the provider is confident that it is plantar fasciitis, then he/she will suggest an appropriate treatment plan for you
- The earlier you start treatment, the better. Early intervention helps prevent the condition from worsening and facilitate a faster recovery.
What Does Treatment Look Like?
Typically, treatment for plantar fasciitis comprises a blend of strategies that can be performed in an office and at home. Among the most prevalent treatment options are:
- Resting and abstaining from activities that exacerbate the condition.
- Applying ice therapy initially to alleviate pain and reduce inflammation. Heat should be used afterwards.
- Photobiomodulation
- Engaging in stretching exercises targeting the plantar fascia and calf muscles
- Opting for suitable footwear
- Utilizing orthotic devices like shoe inserts or night splints to support the foot and relieve pressure on the plantar fascia
- ***It’s crucial to focus on foot strengthening even if you are using orthotics
- ***Understand that these are short-term modalities
- Using them long-term will only set you up with weaker feet and a greater chance of re-injury
- Undergoing physical therapy or other rehabilitation methods to enhance flexibility, strength, and range of motion
It’s crucial to work closely with a healthcare professional to develop a personalized treatment plan tailored to your specific requirements and concerns.
At-Home Modalities
Remember, none of these should be taken as medical advice, and you should use your own best judgment on where to start. You may not need some of these recommendations because your experience may be milder than another’s. Some, however, apply to everyone. My goal is to provide you with all the options in this section.
One important note on rehabilitation in general. The area in pain is not always the cause of it. In the case of plantar fasciitis, anywhere in the lower kinetic chain, from the foot to the low back (but it can even be up to shoulders and neck), could be contributing to its development. Smart practitioners know this, and balancing out the weaknesses in those areas is key!
Hydration
Yep, clean water is a good start regardless. A 2017 study found that those who were dehydrated had less flexibility, reduced range of motion, and more stiffness in the leg muscles. All of which are not good. This includes, of course, the plantar fascia. Clean water is best, ideally free of fluoride. Right now, my favorite two systems are Clearly Filtered and Aquatru. There are pros and cons to each, and the best option for you may come down to where your water is sourced from. The best (and most expensive option) is a full home filtration system. Alternatively, you may have access to healthy spring water, which is also great.
Movement
You will be tempted to rest your feet when they’re aching, but the truth of the matter is we need that liquid crystal water inside our body to move to be at its best. You may notice your heel hurts more in the morning or after a longer period of inactivity. That’s because the plantar fascia has become tight and rigid overnight. Even gentle movement in the morning can help provide relief.
Be smart about it though. You may want to take a break from higher-impact sports, like tennis, basketball, or soccer while recovering.
You do want to be walking (ideally on natural surfaces) at least 5,000 steps per day, if not more, if you can. It may be even more beneficial to walk on a low incline (1-10 degrees) if you are able to.
Walking Barefoot
If your gait mechanics are good, I highly recommend adding barefoot walking to your rehab as soon as possible. Ideally this is done on grass, dirt, or the hard sand next to water. The benefit of natural terrain is that it is uneven, which helps restore the intrinsic muscles of the feet.
Walking barefoot has other amazing effects on the body, but the most overlooked one is the grounding effect. To summarize, the Earth’s surface has a net negative charge, and when you walk on the ground with bare feet, you tap into a virtually unlimited supply of electrons, which act as antioxidants in the body. These antioxidants can help facilitate the healing process.
Pain After Walking? Gas-Pedal Exercise
If you have foot discomfort after walking, consider putting heat on the affected area.
You will also want to consider performing a gas-pedal foot exercise. This increases blood flow to the feet which is vital for healing every structure in the foot.
- While sitting, slightly extend your legs out from your body.
- Plantar flex one foot and dorsiflex the other foot.
- Alternate each foot in dorsiflexion and plantarflexion.
This causes the calf muscles to work, especially the soleus muscle, which is deep to the gastrocnemius. The soleus muscle is incredibly important because it acts as a fluid pump. It also allows for fresh blood to be pumped down into the foot and old used up, deoxygenated blood to be moved away. It also propels the flow of lymphatic fluid upwards.
Cold Therapy
Best used immediately following an injury. Applying ice to the affected foot for 20 minutes 3-4x/day should help lessen plantar fasciitis pain. One study found that cold therapy for 20 minutes at bedtime reduced plantar fascia thickness by 13%, decreased pain by 44% and increased by 86% the amount of force that could be applied to the feet without pain. You can apply cold to the foot with an ice bucket, ice pack, a package of frozen vegetables, or a paper cup filled with water.
However, I recommend heat and not cold after the first 24 hours post-injury. Heat will bring more blood and healing factors to the area in the most need of it.
Stretches
Simple exercises that stretch the plantar fascia and Achilles tendon are key to alleviating plantar fasciitis.
The Achilles tendon is the longest, strongest tendon in the body. Sometimes, when the Achilles is tight, it can put extra strain on the plantar fascia, which can eventually lead to plantar fasciitis. The same can be said for the calf muscles, the gastrocnemius and soleus.
Heel Drops
- Stand on a step with your heel hanging off the edge.
- Let your heel drop down below your toes.
- Hold for 10-30 seconds. Repeat for 8-10 repetitions.
- Hold onto a wall or banister for support if needed.
Wall Stretch (Two Versions: Gastrocnemius & Soleus)
Strong and mobile calves are foundational for a healthy plantar fascia. Guess what a major cause of calf tightness is? Sitting all day! Go figure. Almost every case of plantar fasciitis I’ve seen has tight calf involvement. Don’t skip these stretches.
Gastrocnemius
- Face a wall with staggered feet, and stand about an arm’s length away.
- Keeping the heel of your back leg planted, bend your front knee and slowly lean toward the wall.
- Keep the back leg fully extended, with the heel on the floor.
- Hold for 60 seconds, using long, slow nasal breaths. 4 seconds in, 6-8 seconds out.
- Bring your front leg across your body if you are able for a more advanced version of the stretch.
Soleus
- Face a wall with staggered feet, and stand about an arm’s length away.
- Keeping the heel of your back leg planted, bend your front knee and slowly lean toward the wall.
- Now bend your back knee a bit, with the heel still planted on the floor.
- Hold for 60 seconds, using long, slow nasal breaths. 4 seconds in, 6-8 seconds out.
- Bring your front leg across your body if you are able for a more advanced version of the stretch.
Towel Stretch
This stretch helped lengthen the plantar fascia and the muscles along the bottom of the foot. After strengthening work or a long day on your feet, this stretch is a helpful addition.
- Sit on the ground with your legs extended in front of you.
- Loop a towel or exercise band around the ball of one foot. Hold the ends of the towel in your hands, and pull your toes back toward you to feel a stretch.
- Hold the stretch for 30-60 seconds, using long, slow nasal breaths. 4 seconds in, 6-8 seconds out.
- Repeat 3 times each side.
Exercises
If you want to return to your regular exercise routine, you need to build the tissues to tolerate the loads you are placing upon them.
Remember, the more motion, especially toe motion you can get in, the more you can work those intrinsic muscles of the feet.
Monkey-Foot Towel Lift
Even though plantar fasciitis is characterized by heel pain, the toes play an integral role. Wearing conventional footwear creates poor foot mechanics and weakened foot muscles, which changes the shape of the foot with time.
This is a great exercise to strengthen the arches of the feet and improve foot/toe flexibility. It is also great for those whose feet are too tender to walk outside barefoot.
Creating space and spreading the toes can aid in relieving tension in other foot muscles, alleviating the symptoms of plantar fasciitis pain.
To do this exercise:
- Sit on a chair and position a small towel or cloth on the floor in front of you.
- Keep your heel grounded while using your toes to lift the towel off the floor.
- Release the towel and repeat the movement 10 to 20 times.
- For a more advanced version of this exercise, add weight to the towel by placing a heavy object on it.
- If you work in an office and don’t have a towel available, you can perform this exercise with pens or paper clips.
Heel Raises
You may want to use a wall or the back of a chair for balance when performing this exercise:
- Position your support.
- Place both feet flat on the floor.
- Use the chair for balance as you rise onto your tiptoes, holding the position for five seconds.
- Slowly lower yourself back down.
- Complete two sets of 15 repetitions, resting for 30 seconds between sets.
- For a more advanced version, place a tennis ball between your ankles, and do not let the ball drop as you raise (see pictured above)
You can also perform the eccentric version of this exercise:
- Position your feet on the ground or an elevated surface, approximately hip-width apart, ensuring your knees and toes face forward. Align your feet with your ankles and distribute your weight evenly.
- Engage your calf muscles as you lift your heels off the ground or surface, rising onto your toes.
- With control, lower slowly from the top of the calf raise, counting to five as you lower down.
- Start with 3 sets of 10 repetitions.
- You can increase the intensity by performing these one leg at a time.
Reverse Lunges
Lunges are fantastic for balance and lower body strengthening. As you get stronger, this is an awesome exercise to add to your regimen.
- Stand with your feet hip-width apart.
- Take a step back with your right foot and descend into a lunge, ensuring your right knee comes close to the ground while your left thigh remains parallel to the ground.
- Maintain a straight back and ensure your left knee aligns with your toes.
- Return to the starting position.
- Repeat this sequence on both legs for 3 sets of 12-15 repetitions each.
- Incorporate this exercise into your routine 2-3 times per week.
Photobiomodulation
Red and NIR light exhibit anti-inflammatory properties. What’s great is, unlike anti-inflammatory medications such as NSAIDs, there are no side effects attached! Research has found that light therapy influences various molecules involved in inflammation, including reactive oxygen species, reactive nitrogen species, and prostaglandins.
PBM increases the rate of tissue repair. Light therapy has been shown to speed up recovery post-exercise and improve wound healing, including tendon injuries.
Fringe red light devices are my favorite for at home use.
Night Splint
When we sleep, our feet tend to plantarflex, which contracts the plantar fascia. If you are currently experiencing plantar fasciitis, you may want to consider wearing a night splint while you sleep.
A night splint is a device worn on the foot during sleep to gently stretch the Achilles tendon. Sometimes, these can be uncomfortable when getting started. You may want to try it for 20 minutes or so while you’re still awake to start getting comfortable with it before using it for a full night.
Toe Separators
Modern shoes have narrow toe boxes, which can change the shape of your foot over time. This can lead to foot pain and even plantar fasciitis.
Toe separators are an effective method for stretching the small muscles surrounding the toes and the toes themselves. They are an affordable tool that can significantly reduce pain in the feet and toes, making it particularly beneficial for addressing conditions such as plantar fasciitis.
Chiropractic
Anywhere from the low back and below can contribute to plantar fasciitis. Especially with how often Modern Humans sit, it would be wise to seek out a skilled chiropractor to help you identify any imbalances in the low back that could be adding fuel to the fire. A very common contributor is called “lower cross syndrome.” This can contribute to an anterior pelvic tilt and ultimately poor posture. If there is poor posture, that is going to affect gait mechanics.
Massage
Best in acute situations. I prefer more active modalities in general, but this certainly has its place. There is a more recent study that found five minutes of deep tissue massage helped alleviate plantar fasciitis pain, while also enhancing flexibility and range of motion. My two cents is that these are short-term benefits, but for someone in acute pain, it is useful. There is similar research for calf massage.
Here’s how to perform them…
Plantar Fascia:
- Dorsiflex your foot to pull your toes back.
- Identify the most tender area of your heel. Using one or two fingers, apply firm pressure and massage back and forth across this spot within a 1-inch radius.
- Ensure the pressure is deep enough to move the skin with your fingers, rather than just sliding them across the surface.
Calves:
- Cross one ankle over the opposite knee, exposing your calf.
- Use your thumbs to apply pressure to tender areas along the center and sides of your calves, for approximately 10 minutes.
You can also use a tennis ball or lacrosse ball to massage the plantar surface of the foot.
Acupuncture
While I don’t personally perform acupuncture, I am a major advocate for its use. Research has demonstrated that acupuncture is an effective treatment for plantar fasciitis. It may also reduce the risk of recurrence. When combined with herbal remedies, one study found that acupuncture treatment had a success rate of 91.8%.
Epsom Salt Baths
I will be the first to tell you there isn’t a ton of peer reviewed literature to support this. However, I have seen people do Epsom salt foot baths, and have their plantar fasciitis pain reduced to zero within a day. I have spoken to other practitioners about this, and they have seen it as well. If anything, there is anecdotal support, and there are virtually no downsides to trying.
Epsom salts are known for their skin-softening properties and for reducing inflammation.In theory, the primary component of Epsom salts, magnesium sulfate, is FDA-approved for use as a laxative.
Additionally, research has indicated its effectiveness in treating conditions such as heart arrhythmia, tetanus, and eclampsia. There are also studies that support the use of magnesium for reducing foot pain.
Although there isn’t any peer-reviewed evidence of the effectiveness of Epsom salts specifically for plantar fasciitis, the extensive anecdotal evidence for Epsom salts and foot soaking should not be dismissed.
A long, warm soak in a bath provides your feet with an opportunity to rest and repair, which many podiatrists and medical professionals recognize as crucial for recovery.
Nutritional Support
Magnesium
Magnesium plays many important roles in the body, most notably nerve transmission, muscle relaxation and contraction, and regulation of metabolism. The average human contains about 100 milligrams of magnesium per kilogram of bodyweight. Magnesium can also help prevent calcium deposits in tendons, ligaments, and muscles.
Simply put, if we don’t have adequate amounts of magnesium, muscles and nerves do not function as well as they should. It is found primarily in bones, but can also be found in organs such as the heart, skeletal muscle, kidneys, and pancreas.
Food sources are best. Consider adding more fruits and vegetables, especially dark leafy greens, seaweeds, nuts, seeds, dried fruits, potatoes, bananas, apples, peaches, lima beans, black-eyed peas, sesame seeds, alfalfa, soy products, cereal grains, avocado, millet, oatmeal, peas, figs, and okra.
Vitamin B5 (Pantothenic Acid)
Vitamin B5 is utilized by the body’s adrenal glands to generate cortisol, a natural anti-inflammatory agent. Incorporating Vitamin B5 into treatment regimens can effectively address plantar fasciitis.
The best sources of B5 include peas, royal jelly, green vegetables, avocados, bananas, dried mushrooms, broccoli, collard greens, oranges, legumes, and sunflower seeds.
Vitamin C
Vitamin C plays an essential role in both tissue growth/repair and collagen synthesis. Additionally, it is also a powerful antioxidant, and works in conjunction with vitamin E in enhancing immune system function.
The best sources are all fruits and vegetables, especially citrus fruits, strawberries, blackberries, kale, papayas, mangos, guava, persimmons, apples, watermelon, red chili peppers, tomato juice, sweet potatoes, cauliflower, Brussels sprouts, and broccoli.
Anti -Inflammatory Herbs
Herbs like ginger, turmeric, rosemary, cinnamon, clove, and sage are all great for reducing systemic inflammation. Perhaps a golden milk latte with your favorite plant milk and a ½ tsp each of turmeric, cinnamon, cardamom, ginger and honey, plus a few grinds of black pepper is a nice warming drink that can be helpful! Boswellia Complex by Mediherb, Turmeric Forte by Mediherb, and Inflammatone by Designs for Health have been really useful tools for helping with joint pain in my experience. You can sign up to my dispensary and get them 10% off here.
Prevention
An ounce of prevention is worth a pound of cure!!!
Plantar fasciitis symptoms can be painful and even debilitating at times. That’s why it is vital to prevent it from occurring at all. Here are some highly effective prevention strategies:
- Maintaining a healthy weight alleviates pressure on the feet
- Choose appropriate footwear with a spacious toe box to facilitate natural toe movement
- Even better, go barefoot when you can on natural surfaces
- Slowly increase the intensity and duration of physical activities to prevent overburdening the plantar fascia
- Incorporating breaks into routines and minimizing extended periods of standing or walking
- Mobilization and flexibility are key! Stretching and healthy movement patterns exercises enhance flexibility and mitigate injury risks
Wrapping Up
Although it can be very painful and annoying, plantar fasciitis is mostly preventable and highly treatable with rest, icing, massage and targeted stretches and exercises. Symptoms usually go away within several weeks or months and only very rarely are interventions including medications and surgery needed.
Just like with exercise, you will see results when you have the right intentions and are consistent.
You take care of your feet, and your feet take care of you. While often overlooked, foot health is an essential part of general health and well-being.
Anyone who has gone any period of time not able to walk can attest to this. With proper care and attention, you can keep your feet healthy and pain-free for years to come.
Until next time,
Dr. Vincent Esposito
Want More?
Whenever you’re ready, there are two ways I can help you:
- If you are not getting energizing, restorative sleep every single night, then you’re missing out on the single most important recovery tool. But I have a solution, my book: How to Get World Class Sleep! If you’ve struggled with insomnia, have trouble falling asleep, or wake up feeling sluggish, then this is for you! Fall Asleep Faster. Recover More Quickly. Wake Up Refreshed! Find it here!
- I take a comprehensive, individualized, one-on-one approach with every single person I work with. Perhaps you have tried so many different routes to better yourself, but not see the progress you desire. If you want clear action steps and a guide to help you lay the foundation for healing and feel confident in your body, this is for you. If you want a partner who is committed to helping you master your own wellness, then schedule a FREE 15-minute call with my team to apply to get your health on the right track.